Public health, explained: Sign up to receive Healthbeat’s free national newsletter here.
California’s new initiative to compel treatment for some of the state’s most severely mentally ill residents — many of whom are living on the streets — is falling short of its initial objectives. But with the program expanding from 11 counties to all 58 on Dec. 1, state officials are projecting confidence that they can reach their goal to help 2,000 adults by the end of the year.
In the first nine months of CARE Court, 557 petitions were filed by first responders, families, or local health officials, all of whom can now request help for individuals who are ill. As of the end of June, 100 people had been placed in court-approved treatment plans, according to the latest data available.
“We’re pleased to see how many people have come through and how appropriate those referrals have been so far,” said Corrin Buchanan, a deputy secretary for the California Health and Human Services Agency, which oversees the program. “These are the right kinds of people we were hoping to serve.”
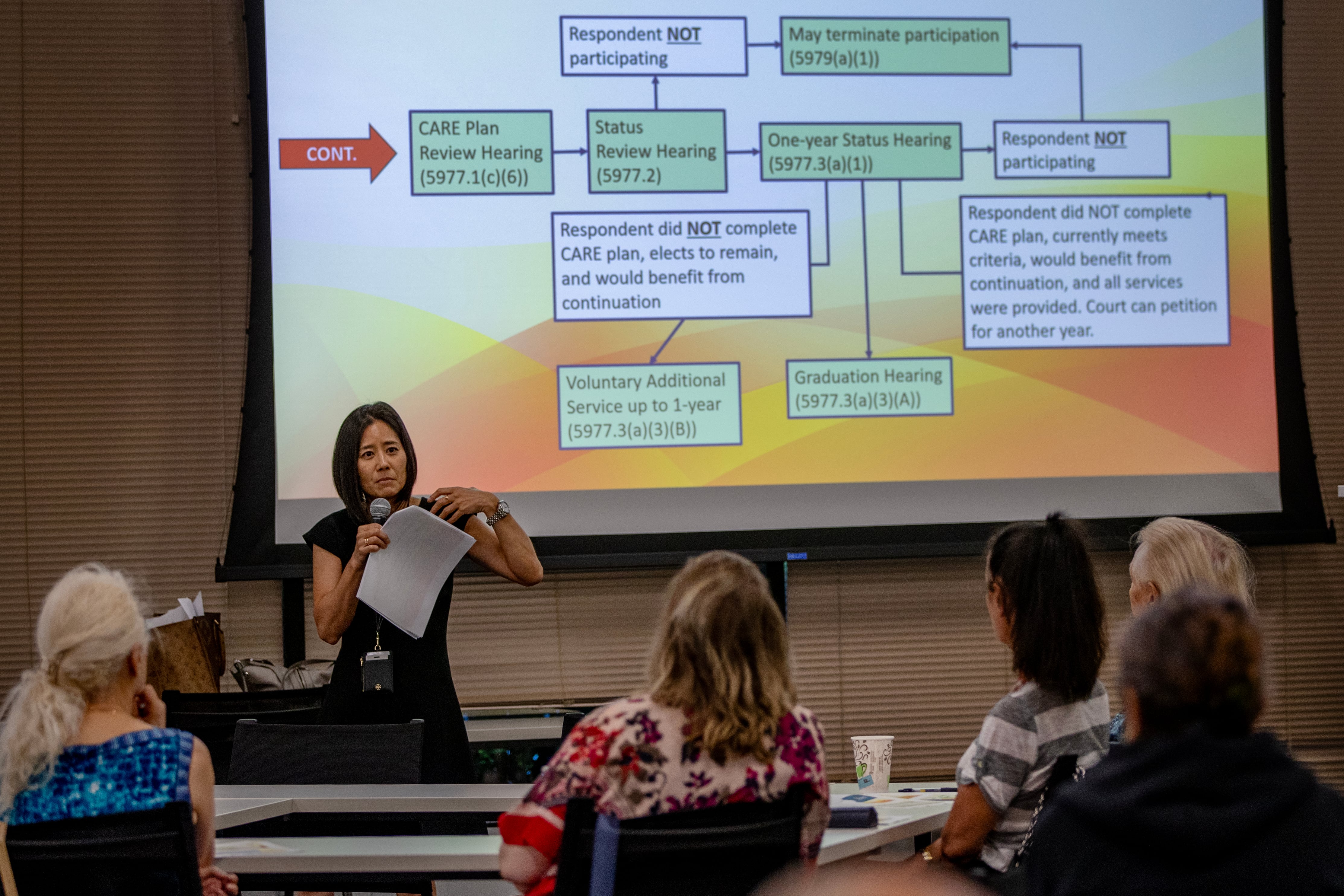
The Community Assistance, Recovery and Empowerment Act — the first law of its kind in the nation — empowers civil court judges to order adults into monitored plans that include housing, social services, and treatment for addiction or mental illness. Until now, counties such as Los Angeles, San Diego, and San Francisco have been piloting the program, which Democratic Gov. Gavin Newsom has called a “paradigm shift” to prioritize the Californians who are sickest and most in need.
But officials in counties that have launched the program said the low number of cases reflects the amount of time it takes — sometimes weeks or months — to find people and persuade them to enroll. And judges dismissed nearly 40% of petitions in the program’s first nine months, in part because of the program’s narrow criteria to target only those with untreated schizophrenia or other psychotic disorders.
State officials have estimated that between 7,000 and 12,000 people will be eligible for a CARE plan. The state has directed $358 million in one-time funding, and it projects it will spend $108 million a year on the program.
Treatment through CARE Court is voluntary
CARE Court is one of a raft of changes Newsom has spearheaded to address rampant homelessness, including overhauling the public mental health system and funneling billions of dollars for counties to execute those changes on the ground. Recent moves include loosening conservatorship laws and passing Proposition 1, a voter-approved measure that gives the state more control over mental health funding previously managed by counties.
Local health representatives say they’re juggling the governor’s initiatives as he demands results to reduce homelessness.
While CARE Court was meant to target people who cycle in and out of jails and hospitals and onto the streets, county officials said they’re encountering a substantial number of clients who have housing and, in some cases, private health insurance.
Many family members have had their hopes dashed when they find that only a small number of people qualify for CARE Court resources and that ultimately treatment is largely voluntary, county officials said. Unlike in a conservatorship, which hands all decision-making power over to the state or an adult guardian, counties can’t treat or medicate participants against their will. But counties can rack up steep court fines if a judge determines the county hasn’t provided help.
“There’s been a tremendous need for the management of expectations, especially with family members,” said Amber Irvine, program manager for San Diego County’s CARE Court. She added that while she considers the program a success, “we need to, as a whole, adjust our expectations of what can be accomplished in a year with such a complicated program and such a complex population.”
San Diego County’s program has been among the most robust, with 221 petitions filed since it launched in October 2023, although a third of the county’s participants were already under conservatorship. Irvine said 76 of the state’s 100 CARE plan participants are from the county.
But it’s not easy. It takes county outreach workers there an average of 54 days of casual conversations, encounters in encampments, and distributing food or supplies — activities the state doesn’t typically reimburse for — to persuade someone to accept services. In some cases, that number stretches to more than four months, Irvine said.
She and others credit the state for funding CARE programs, which has enabled county staff to conduct intensive outreach. San Diego County boasts the state’s first CARE graduate, a participant who was able to exit conservatorship and leave a locked psychiatric facility.
Though Irvine thought the county was overprepared with 15 new hires, the staff was able to take on less than half the anticipated caseload. Other counties have had to shift personnel from understaffed departments to prepare for CARE Court.
Staffing needs remain uncertain with the remaining counties set to launch CARE programs, said Jacqueline Wong-Hernandez, chief policy officer for the California State Association of Counties. In September, Newsom vetoed a bill that would have provided scholarships to mental health professionals if they agreed to work for CARE Court, citing budget pressures.
Alameda County’s contractor has prepared for the Dec. 1 launch by hiring a team of more than a dozen, including a full-time nurse, case managers, employment coordinators, and a clinician to prescribe medications.
Counties struggle to implement multiple initiatives
Officials there are identifying clients already known to cycle through crisis services, so they can file petitions on their behalf. And the county is figuring out how to tap state housing funds that allow clients to stabilize in short-term housing.
“It’s really a lot to set up,” said Kate Jones, who is helping to oversee the county’s rollout.
Mark Ghaly, who was the chief architect of the CARE program before leaving his post as California’s health secretary this fall, said he worked for many years at the county level and empathizes with counties struggling to implement multiple initiatives at the same time. He added that CARE Court was never meant to be launched in a vacuum.
“We’re going to have to see this whole tapestry of efforts come together to really make the kind of dent that I know we can as a state,” Ghaly said.
State Sen. Tom Umberg, a Democrat who co-authored CARE Court legislation, said that more health care providers need to be made aware of the program so they can help spot potential enrollees.
Still, one county representative worries that the public could conflate court-approved treatment plans for the severely mentally ill with solving homelessness. In 2023, California had an estimated homeless population of more than 180,000.
“The solution to homelessness in California is housing, and the more people are prevented from falling into homelessness in California, the fewer county behavioral health clients we will have,” said Michelle Doty Cabrera, executive director of the County Behavioral Health Directors Association of California.
Christine Mai-Duc is a reporter for KFF Health News, Healthbeat’s national reporting partner.