Public health, explained: Sign up to receive Healthbeat’s free Atlanta newsletter here.
When Jimmy Carter started his nongovernmental organization in Atlanta soon after leaving the White House, he reached out to his former CDC director to run it.
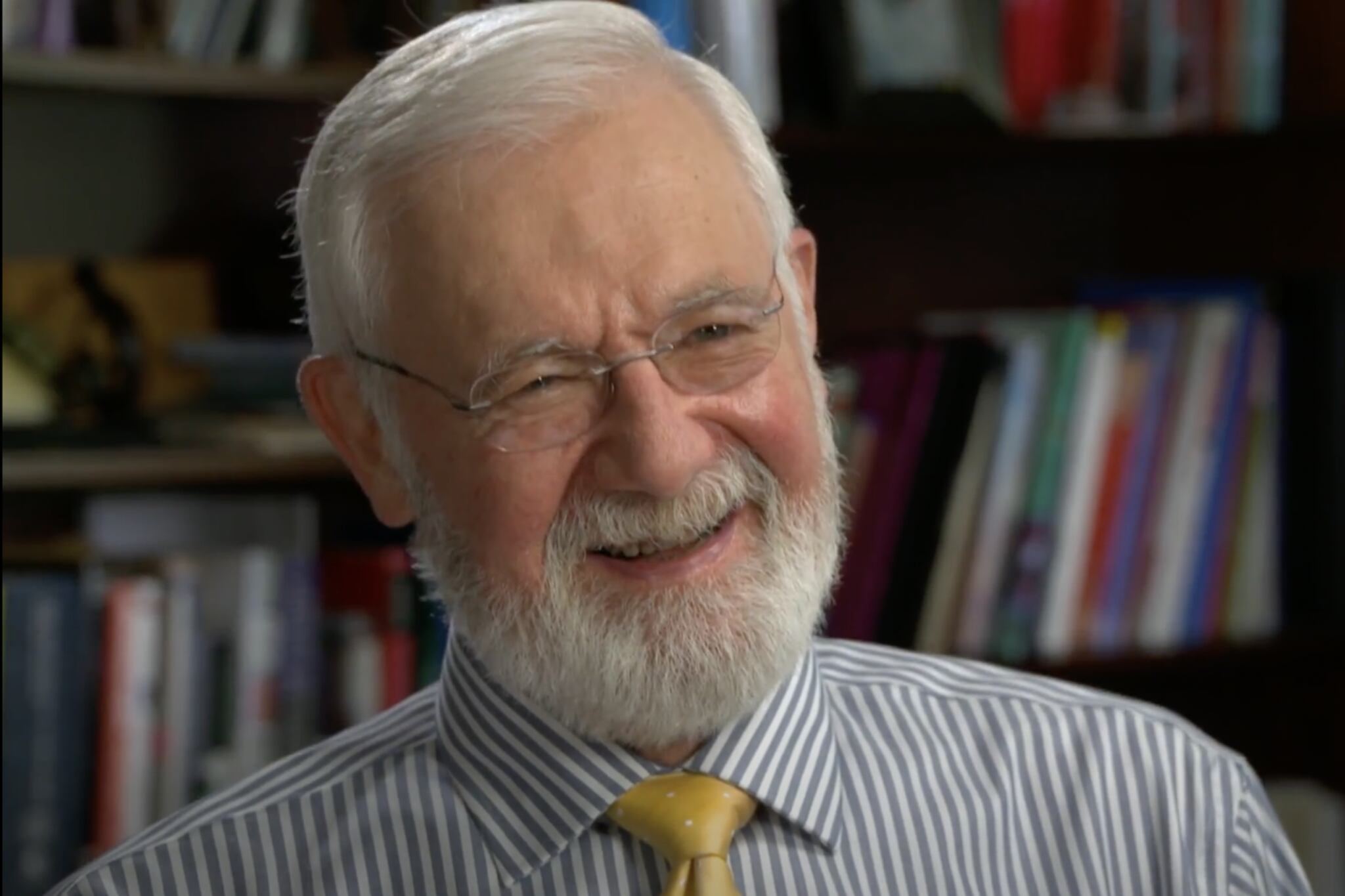
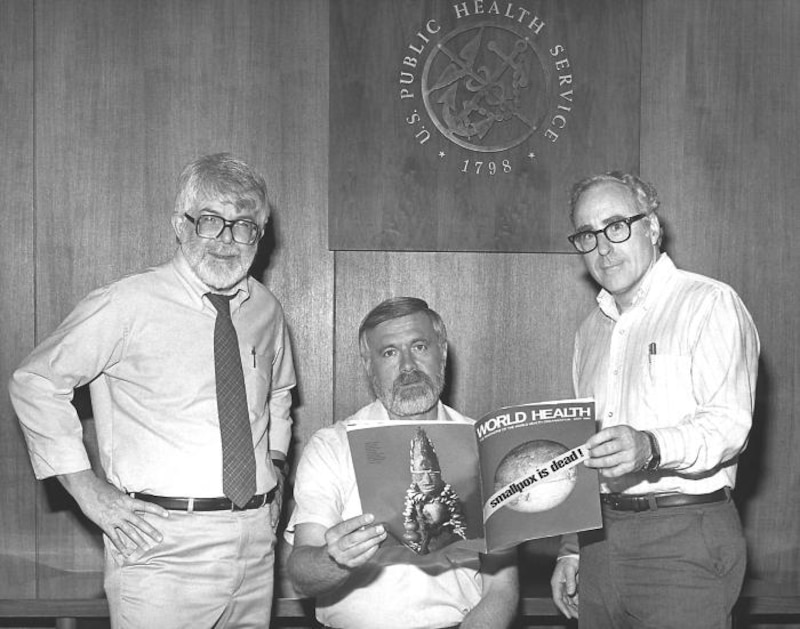
Dr. Bill Foege, who after leaving the Centers for Disease Control and Prevention launched what became The Task Force for Global Health, was known for his role in leading the eradication of smallpox in the 1970s. He wasn’t ready to give up his global public health work.
“‘Would it make a difference if I also became interested in global health?’” Carter asked Foege.
It made all the difference. In the ensuing decades, the Carter Center was credited with public health improvements around the world, fighting diseases like malaria, river blindness, and Guinea worm.
As Carter is laid to rest this week after his Dec. 29 death, Foege, 88, spoke with Healthbeat about his work on public health with Carter, his worries about the incoming Trump administration, and how to help win people’s trust in science.
The conversation has been edited for length and clarity.
What do you consider President Jimmy Carter’s public health legacy to be?
When he first approached me about being executive director at the Carter Center, I had real reservations. I told him I spent my life in global health. There aren’t enough people working in global health, and this was quite some time ago, and it was true, and I said it just didn’t seem right for me to leave it.
He came back a day or so later and said, “Would it make a difference if I also became interested in global health?” And of course, it’s incredible to have that sort of opportunity.
What he did was demonstrate to me what we should know, which is public health people and politicians have to work together because we’re totally dependent on appropriations that come from politicians making decisions on what they will fund. Sometimes you see public health people very distressed that politicians are involving themselves. Yet there’s no option; we have to get them involved, not just in appropriations, but to have them invested in a health outcome. And that’s what President Carter could do.
If I went to Africa, I could probably quite easily get an appointment with the minister of health. I could not get an appointment with the minister of finance, and they’re the crucial ones, and I certainly could not get an appointment with the head of state.
President Carter would go right to the head of state. Head of state would get a Cabinet meeting, including the minister of health and the minister of finance. When Carter would sell him on onchocerciasis [river blindness], or Guinea worm, or schistosomiasis, or other things, and the head of state would say, “This is something we want to do,” the minister of health and the minister of finance are going to just trip all over themselves to please the head of state. He showed what a politician could do working with public health.
What is the most effective thing public health leaders can do to build trust in their work and in science?
I often use the word trust because it’s the glue that holds together a coalition. It was certainly the glue that held together the coalition in India, as we were doing smallpox eradication.
With public health, there are three things that I often tell public health students that [they must do] in order to get trust.

Number one, start with the best science. We’ll all make mistakes on science. No question about that. Admit them when you find them, go back and correct them and continue to do the best science possible. And [British biologist Thomas] Huxley once said that science is simply common sense at its best, that it’s not anything that people can’t understand. Nowadays, there are people who think they can’t understand science, and therefore they don’t trust it. No, it’s just common sense at its best. We have to become better at describing the science so that people do understand it.
Number two, add art. The first scientist that we know in history was an Egyptian by the name of Imhotep. He was a physician, but he was also an architect. He designed the step pyramid, and then he supervised the building of the step pyramid. The reason this is important is it brings creativity into the process. Instead of just common sense at its best, you have creative common sense at its best.
And then, the third ingredient: I go back to Roger Bacon, who about 800 years ago, was asked to do a summary of science for the pope. And it’s been 50 years since I’ve read that, but I still remember so clearly that he said, “Science has no moral compass.” It means you have to provide scientists with a moral compass in order to bring all three of these together for moral, creative common sense at its best. That’s the way we regain trust — by keeping those things in mind.
What is your biggest worry about public health right now?
You hit it with the trust issue. The public health people have to take this very seriously, and this is part of why we have to reach out to politicians. We need them to fund our projects, and if they don’t fund the projects, then we can’t provide what we should to the public. I’m very concerned about this anti-science, anti-government movement, the anti-vaxxers, for instance.
The first vaccine that we have was developed by Edward Jenner in 1796. The first anti-vax group developed in 1796. This is an old, old problem. Because the smallpox vaccine was taken from cowpox, they would make cartoons of people who had the head of a cow growing out of their arm to warn people not to get vaccinated.
This anti-science, anti-government movement has to be countered with good information. Parents are not trying to hurt their children when they keep them from being vaccinated. They believe that the vaccines are harmful, and why shouldn’t they? Because now they don’t have the disease and the risk of the disease to compare to the risk of the vaccine. When I was young, you had no trouble convincing people to take the polio vaccine, because they saw what happened, the crippling of polio. You had no trouble in Africa getting people to take the measles vaccine, because 7% of all children were dying of measles in Africa.
Now you don’t have the disease, so people can’t make that comparison, and they only look at the risk of the vaccine, and they forget that the risk of the disease has gone down because of a social contract that we all have. The problems are gigantic, there’s no question about it. We have to be so careful about presenting the best information and figuring out how to get the grass roots to solve this on their own.
How do you expect public health to change under the new Trump administration? What do you tell colleagues who are worried about Trump’s policies or the officials he’s choosing?
I worry about what could happen over the next four years, and I worry about some of these ideas of stopping polio vaccines. Polio will come back.
We were at a very low point with measles. When I started working in Africa in the ’60s, 7% of children were dying of measles. The introduction of the measles vaccine was unbelievably important, and it went down from 3 million children a year dying of measles in the world to 2 million to 1 million to half a million, and we were down to about 100,000 – still far too many. But now measles is resurging in places because people are worried about giving the vaccine, or they’re competing with Covid and other things. There’s a real task for public health, and I worry about what will happen in this country.
We went through the ’90s and the early 2000s with almost no cases of the usual childhood diseases, but they’ve started coming back.
Why should Americans care about global public health?
Every place in the world is both local and global simultaneously, so no matter where you’re working on public health, you’re working on global public health.
You have one objective, which is global health equity. Those three words, you can’t take any of those three away and have it mean the same thing, and you can add 200 and not improve on it. Global health equity is the objective, and everyone working in public health is doing that.
Rebecca Grapevine is a reporter covering public health in Atlanta for Healthbeat. Contact Rebecca at rgrapevine@healthbeat.org.