Sign up for Your Local Epidemiologist New York and get Dr. Marisa Donnelly’s community public health forecast in your inbox a day early.
Last month, the March of Dimes released its annual report on maternal and infant health in the United States. New York did not score well — a C+ in preterm births, with almost 1 in 10 babies in New York born preterm.
And it’s not just the health of the babies scoring low. Maternal mortality is a huge problem. Two to three women die of pregnancy-associated factors each week in New York, on average. The majority of these deaths are preventable.
Let’s dig into the data to understand how New York is addressing this crisis.
How do we know these stats? All pregnancy-associated deaths are reviewed in New York.
In 2019, New York passed a law requiring all pregnancy-associated deaths to be thoroughly reviewed. Two maternal mortality review boards were formed — one for New York City and one for the rest of the state.
For each pregnancy-associated death, the boards assess preventability, underlying causes, and contributing factors, and then submit a report every other year to identify where and how we must make changes. The most recent reports were released earlier in 2024 using data from 2018-20 (our most recent data).
Maternal mortality in New York state is lower than the national average but still high.
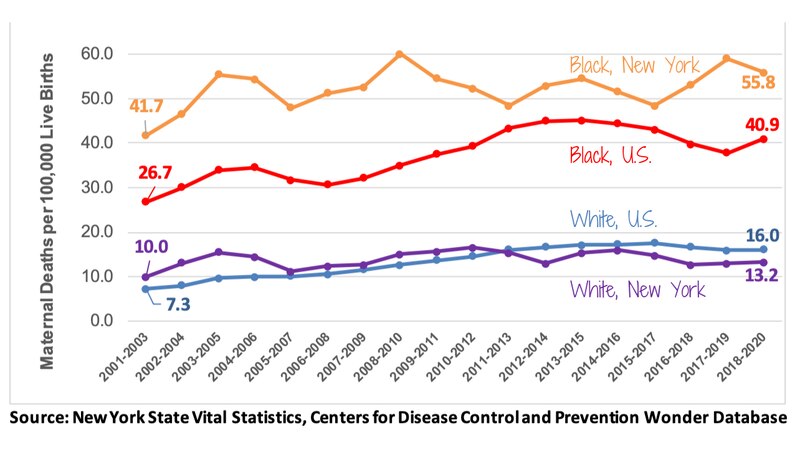
The United States has the highest maternal mortality of all other high-income countries and is one of the only countries where it has risen since 2000. There are also tremendous disparities as to who is most at risk — Black women in the United States die at more than double the rate of white women. Maternal mortality is a public health crisis.
In 2010, New York ranked 46th of 50 states for maternal mortality — meaning New York had some of the highest maternal deaths. In the most recent report, New York is down to 15th.
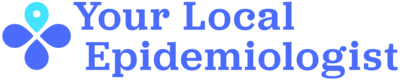
The reports show that from 2018 to 2020, there were 386 pregnancy-associated deaths in New York. While maternal mortality in New York state has remained relatively stable, significant progress has been made in New York City. Still, we have a long way to go to reach the Healthy People 2030 goal of getting down to 15.7 deaths per 100,000 live births. (For comparison, the U.S. maternal mortality ratio is more than 1.5 times higher than in the United Kingdom — 20.4 vs 13.4 per 100,000 live births.)
In New York, the risk is not uniform.
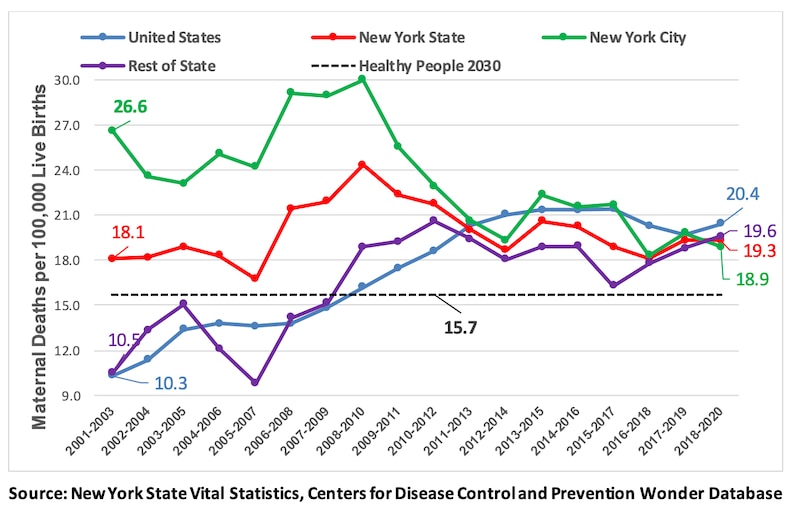
Black women in New York are five times more likely to die when pregnant (or soon after delivery) compared with white women.
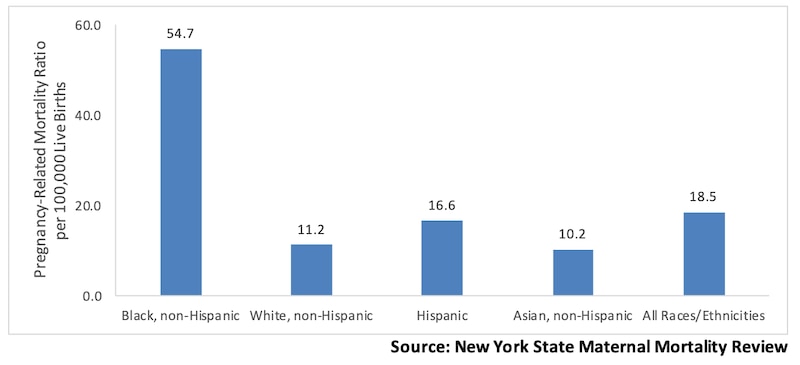
Disparities are also seen in infant health. The infant mortality rate for babies born to Black mothers is 2.4 times the average New York state rate.
There has been little improvement in these gaps over the past two decades. Mortality for Black pregnant women in New York has consistently remained higher than the national average for Black pregnant women.
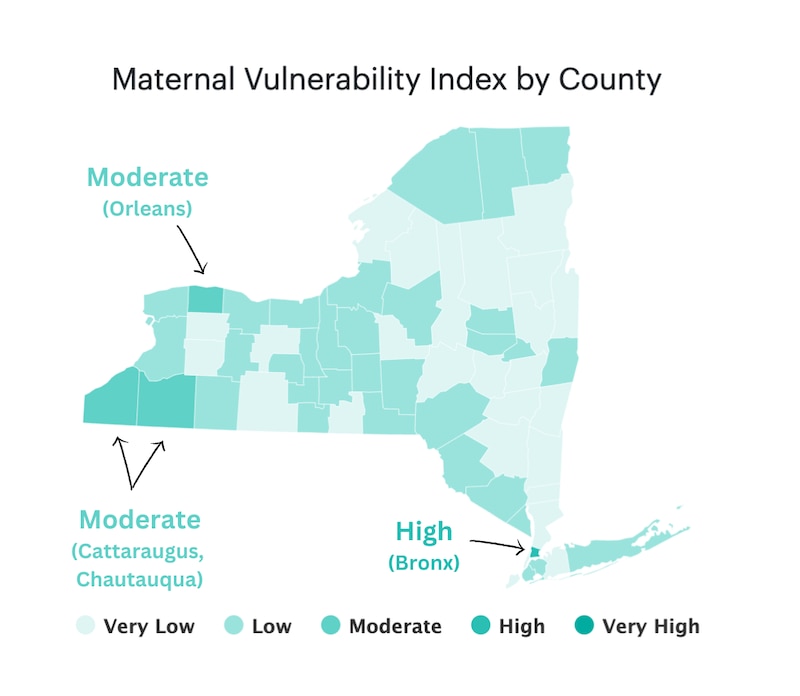
There are also stark disparities based on where pregnant women live in New York. Maternal vulnerability (a mom’s risk of poor health outcomes during pregnancy) is highest in the Bronx, Orleans, Cattaraugus, and Chautauqua counties.
What is causing these high mortality rates, and why are there such substantial disparities?
Bleeding, strokes (embolism), and mental health conditions (including overdoses) are the leading medical causes.
- Overdose has recently emerged as a leading cause of pregnancy-associated death. From 2016 to 2020, 14% of pregnancy-associated deaths in New York City were due to overdose, with the vast majority involving an opioid. For context, around 4% of deaths in New York state are due to overdose.
Chronic health conditions are also significant risk factors for poor maternal health outcomes and preterm delivery. Nationally, women with diabetes had a preterm birth rate of 28.8%, and women who had high blood pressure had a similar rate (23.3%).
Discrimination was a probable or definite circumstance for 47.1% of pregnancy-related deaths in New York. This includes the following:
- Structural and systemic discrimination, like how care and services are harder to access for people living in low-income communities
- Individual discrimination, like not taking patient complaints seriously or dismissing them as normal discomfort due to race, gender, education status, income status, etc.
What is being done to address the maternal mortality crisis in New York?
Public health efforts have to be hyper-focused and evidence-based:
- Ensure access to doulas. Doulas are professional perinatal coaches who support pregnant people one-on-one and have been shown to improve pregnancy outcomes. Anyone enrolled in New York State Medicaid can receive doula services at no cost during pregnancy and up to 12 months after, regardless of pregnancy outcome. More information and a doula directory are available here.
- Plans of Safe Care to support moms, babies, and families affected by substance use. After screening for substance use and mental health conditions, federal law requires that providers develop personalized plans to identify how a provider, family, and community can support the safety and well-being of the baby and mom. These plans address basic needs, identify support systems, and connect moms to their needed resources. More information on safe care plans is available here.
Gov. Kathy Hochul recently signed legislation to expand coverage and make care more affordable in New York state during and after pregnancy. The new laws include the following:
- Permit pregnant women to enroll in health insurance policies at any time without any extra charges or fees. (Before, companies could charge fees for enrolling due to pregnancy.) Resources are available here.
- Require commercial health insurers in New York to cover prenatal vitamins when a health care provider prescribes them.
- Offer paid prenatal care leave starting Jan. 1, 2025, in New York. More information is available here.
Are these initiatives working?
It’s hard to tell. The data give mixed signals. On one hand, New York has improved its maternal mortality rankings in recent years. On the other hand, the Centers for Disease Control and Prevention estimated that maternal deaths in New York increased by 33% during the pandemic. Many initiatives are just beginning, so time will tell how effective they are.
Bottom line
The health of a health system can be measured by how well it cares for expecting moms. Maternal deaths have profound ripple effects on families and communities and provide an important window into broader health disparities. The loss of any expecting or new mother is a tragedy. We have a lot of work to do to keep our New York mothers and babies safe.
Love,
Your Local Epidemiologist
Dr. Marisa Donnelly, a senior epidemiologist with wastewater monitoring company Biobot Analytics, has worked in applied public health for over a decade, specializing in infectious diseases and emerging public health threats. She holds a PhD in epidemiology and has led multiple outbreak investigations, including at the California Department of Public Health and as an Epidemic Intelligence Service Officer at the Centers for Disease Control and Prevention. Marisa has conducted research in Peru, focusing on dengue and Zika viruses and the mosquitoes that spread them. She is Healthbeat’s contributing epidemiologist for New York in partnership with Your Local Epidemiologist, a Healthbeat supporter. She lives in New York City. Marisa can be reached at mdonnelly@healthbeat.org.







