Sign up for Your Local Epidemiologist New York and get Dr. Marisa Donnelly’s community public health forecast in your inbox a day early.
I’m back on the public health beat in New York after taking a vacation in Hawaii. (Take me back to snorkeling 🐠 and mai tais🍹please!)
A lot happened in New York public health this week. From bird flu in cats to rabies in raccoons, here’s what you need to know.
Bird flu in two New York City cats
Earlier this month, two cats from separate households in New York City tested positive for bird flu. Both died. The likely source of infection? Raw pet food.
The Food and Drug Administration has said uncooked and unpasteurized pet food from cattle or poultry — think raw meat, eggs, or unpasteurized milk — can make pets sick with bird flu. Both New York City cats that died ate raw, canned chicken from Savage Cat Food.
Since 2022, more than 100 domestic cats nationwide have been infected with bird flu, and their infections have been particularly bad. Most have died. (Though they may have been more likely to be tested because of serious illness). The risk of cat-to-human transmission is low but possible — in 2016, a veterinarian was infected with a different type of bird flu (H7N2) after treating a sick cat.
For dog lovers, it’s worth noting bird flu doesn’t seem to be as common or severe in dogs. One study found signs of infection in hunting dogs with a lot of contact with waterfowl, but the dogs did not have serious symptoms.
What pet owners need to know
- Avoid feeding pets, especially cats, raw meat, raw milk, or uncooked eggs.
- Avoid letting pets roam where they are exposed to wild animals. Cats can get infected by exposure to wild birds, animals, or animal droppings.
- Contact your veterinarian if your pet becomes ill after eating raw meat or dairy products. Call ahead so that the veterinarian can be prepared when you arrive.
New York and FDA monitoring for bird flu in raw milk cheese
New research from Cornell University and the FDA found bird flu survived the 60-day aging process in raw milk cheese. While no bird flu has been found in cheeses sold in retail markets, and no human cases have been linked to eating raw cheese, this raises questions about food safety.
Raw milk cheese is made with unpasteurized milk. In the United States, cheese from raw milk must be aged for at least 60 days to reduce pathogen risk. The aging process creates a more difficult environment for bacteria to grow (higher acidity, salty environment, less moisture). This study suggests that it’s not enough to rid cheese of active bird flu virus.
Monitoring will be key to ensuring that our cheese supply remains safe:
- FDA will continue sampling at least 300 cheese products nationwide, including aged raw milk cheeses, as part of its ongoing surveillance system.
- New York participates in the National Milk Testing Strategy led by the USDA. We’re one of 28 states testing raw milk for H5N1.
What you need to know
- Most cheeses in our markets are made from pasteurized milk and are safe to consume. Raw milk products are higher risk, not just for bird flu but also for other bacteria that can make you sick.
- Check labels to know if the cheese has been made with raw milk. There is no federal requirement to label whether raw or pasteurized milk was used, but many cheeses label it in the ingredients. Restaurants should also know, too, if you ask.
Rabies in Suffolk County
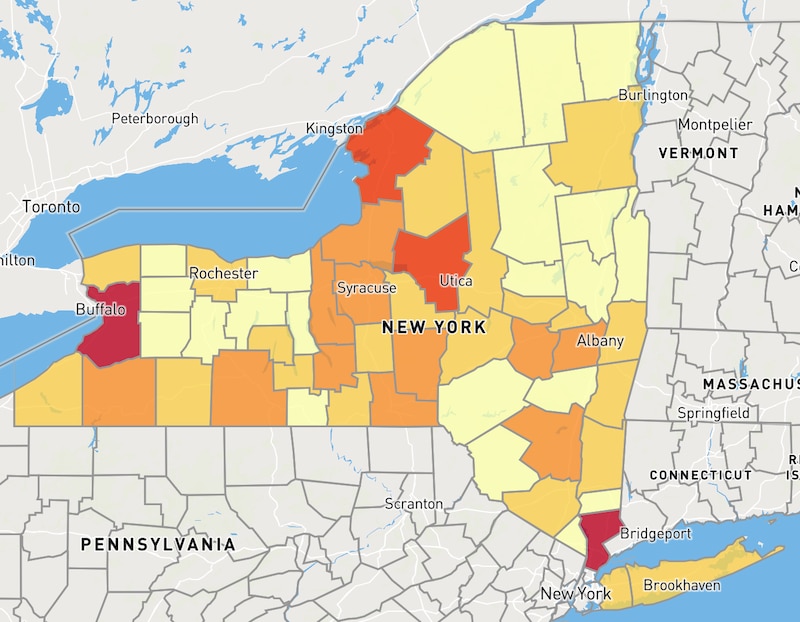
Rabies, nearly 100% fatal for humans, circulates in the wild animals around us. For the first time since 2009, rabies has been detected in Suffolk County raccoons: Two have tested positive since January.
However, this shouldn’t be too worrisome for a few reasons:
1-Rabies is common in New York wild animals. New York state frequently leads the nation in the number of rabid animals. (A raccoon rabies outbreak hit New York in the ‘90s, spreading rabies in wild animals across the state.) Infections are most common in raccoons, bats, skunks, and foxes. Among domestic animals, cats are most frequently diagnosed in New York.
2-We have tools to help.
a. Wildlife: We reduce wild animal rabies by vaccinating wildlife. Many communities, including in New York, distribute baits containing oral rabies vaccine across parks and wooded areas (sometimes using helicopters). When raccoons and other animals eat the baits (which smell like fish), they become immunized, protecting them against rabies.
b. Pets that come into contact with wild animals are at greatest risk of rabies. All cats, dogs, and ferrets should be vaccinated for rabies—in New York, state law requires it. Unvaccinated dogs or cats that are exposed are required to be euthanized or isolated for up to 6 months under observation.
c. Humans: People who work directly with animals have occupational risk, and should be vaccinated for rabies. People who may have been exposed to rabies (through an animal bite or scratch) will need post-exposure prophylaxis of the vaccine (getting vaccinated after exposure).
Vaccination and post-exposure prophylaxis have made human rabies rare: We see just 1 to 3 cases in the United States annually. Still, animal bites are common. About 60,000 Americans need post-exposure prophylaxis following an animal bite annually. Thanks to vaccination, New York City hasn’t seen a single human rabies case since 1947.
What you can do
- Ensure that your pets are vaccinated for rabies. All New York counties offer free rabies vaccination clinics. For more information, contact your local health department.
- Do not touch or get close to wild animals, including feral cats. If you are bitten, immediately wash the wound with soap and water and contact your medical provider. Advise children to immediately tell an adult if they are bitten or scratched by an animal.
- If you see a wild animal that doesn’t look well or encounter a dead animal, contact your local health department or 311 if you are in New York City. Rabies symptoms in animals include tiredness, confusion, difficulty moving, aggression, drooling, and chewing objects like wood, soil, or stones.
Getting vaccinated is crucial if a wild animal bites you. I learned that firsthand in college when a monkey bit me while I was traveling — and I’m thankful I got the shots.
Bottom line
The health of our furry friends plays a big role in our community health, even in urban centers like New York City. Consuming raw animal products (milk, meat, eggs, etc.) is risky for people and animals alike. And rabies remains a deadly threat to us and our pets. But keeping pets vaccinated, practicing good food safety, and talking to a provider if you’re exposed or bitten can protect you, your family, and your pets.
Love,
Your Local Epidemiologist
Dr. Marisa Donnelly, a senior epidemiologist with wastewater monitoring company Biobot Analytics, has worked in applied public health for over a decade, specializing in infectious diseases and emerging public health threats. She holds a PhD in epidemiology and has led multiple outbreak investigations, including at the California Department of Public Health and as an Epidemic Intelligence Service Officer at the Centers for Disease Control and Prevention. Marisa has conducted research in Peru, focusing on dengue and Zika viruses and the mosquitoes that spread them. She is Healthbeat’s contributing epidemiologist for New York in partnership with Your Local Epidemiologist, a Healthbeat supporter. She lives in New York City. Marisa can be reached at mdonnelly@healthbeat.org.







